Cryptococcal meningitis
Cases of fatal CM and disseminated cryptococcal infections have been reported with another S1P receptor modulator1
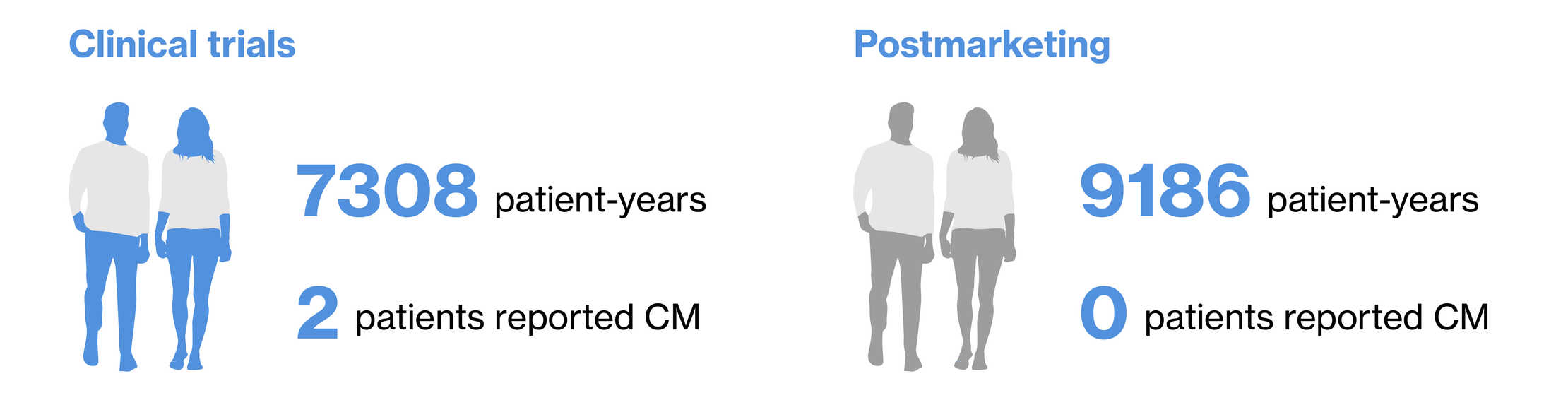
Clinical trials
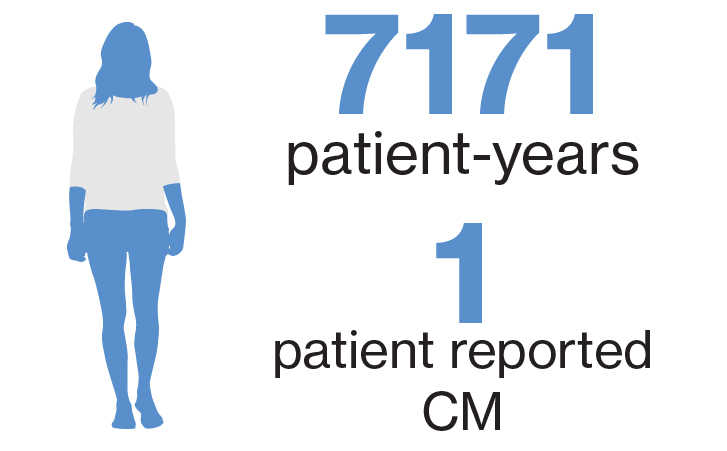
As of 25-September-2020, with cumulative clinical trial exposure of 7171 patient-years, one case of CM* has been reported2
Postmarketing
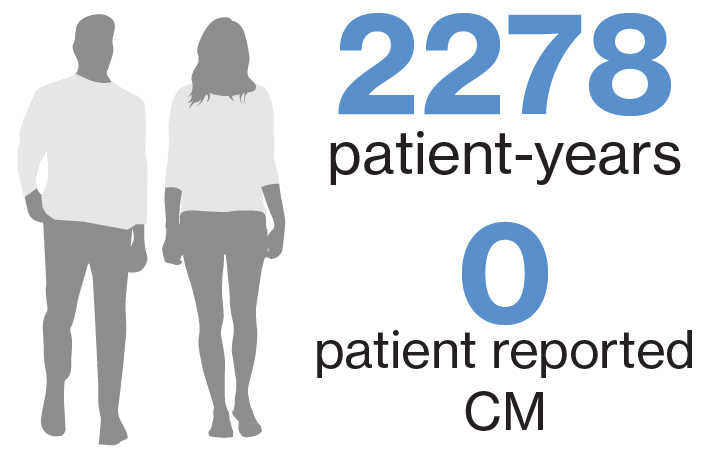
As of 25-September-2020, with cumulative post marketing exposure of 2278 patient-years, no cases of CM have been reported3
*A 62-year-old female patient with long-standing history of MS treated with siponimod for approximately 2.5 years was diagnosed with CM and completely recovered with systemic anti-fungals
About CM
CM background
- Cryptococcosis is a pulmonary or disseminated infection acquired by inhalation of soil contaminated with the encapsulated yeast Cryptococcus neoformans or C. gattii1,4
- After inhalation, Cryptococcus may disseminate frequently to the brain and meninges, typically manifesting as microscopic multifocal intracerebral lesions4
- CM signs/symptoms result from cerebral edema and include nonspecific symptoms such as headache, blurred vision, confusion, depression, agitation, and other behavioral changes. Except for ocular or facial palsies, focal signs are rare until relatively late in the course4
- CM diagnosis is suggested by symptoms of an indolent infection in immunocompetent patients and a more severe, progressive infection in immunocompromised patients and unexplained progressive brain dysfunction, particularly in those with depressed cell-mediated immunity4
- Chest x-ray, urine collection, and lumbar puncture are frequently the initial diagnostic tests done
- Elevated CSF protein and a mononuclear cell pleocytosis are usual in CM
- The latex test for cryptococcal capsular antigen is positive in CSF or blood specimens or both in >90% of patients with meningitis and is generally specific
- General recommendations for CM management4
- Amphotericin B, flucytosine, and fluconazole are antifungal medications shown to improve survival in patients with cryptococcal infections4
